3-in-1 protection while you travel
A combined diphtheria, tetanus & polio vaccine is used for immunisation against diphtheria, tetanus & polio. These diseases have previously had devastating effects throughout history, with many fatalities and life-long health complications.
Nowadays, these diseases are very rare, particularly in the UK and this is thanks to effective childhood vaccination programmes. For this to remain the case, it is important for the diphtheria, tetanus & polio vaccine to continue being part of the routine childhood vaccination schedule.
In many other countries these diseases are still prevalent and anyone travelling to these areas should consider the vaccine. One of our pharmacist can advise you on which countries recommend a diphtheria, tetanus & polio vaccine for travel purposes.
The vaccine we use to immunise against diphtheria, tetanus & polio is Revaxis which provides protection against diphtheria, tetanus & polio. It is specifically intended as a booster and should not be given as the primary course and/or to children under the age of 6. The diphtheria, tetanus & polio combined vaccine is a provided in a single injection. A booster is required every 10 years.
The good news is, protection has never been easier. Health Plus Pharmacy make the diphtheria, tetanus & polio vaccination convenient and accessible for all the community in Cardiff and Pontypool. Book an appointment with your local Health Plus Pharmacist to keep you safe.
Check the risks of a country you’re travelling to on the TravelHealthPro website
About the diphtheria, tetanus & polio vaccine
Price: £35 per dose of the diphtheria, tetanus & polio vaccination
Doses per course: 1
Price per course: £35
When to get vaccinated: You should get your diphtheria, tetanus & polio booster two weeks before travel.
Course: If you have had the vaccine before, you will need one dose as a booster. If it’s your first jab, you may need several doses.
Boosters: How long does the diphtheria, tetanus & polio vaccine last? The vaccine protects you for 10 years. You will need a booster to remain protected after 10 years.
Who to get vaccinated: We offer the vaccine for children from the age of 10.
How it is given: The diphtheria, tetanus & polio vaccine is given as an injection in the upper arm.
Side effects: You may experience mild side effects such as soreness at the injection site or feeling unwell.
Risk if you contract diphtheria, tetanus & polio: Diphtheria, tetanus & polio are serious illnesses which can cause a range of complications. They can be fatal.
About the diphtheria, tetanus & polio vaccination
When given as a booster prior to travel, the diphtheria, tetanus and polio vaccine requires only one injection. If you last had this vaccine more than ten years ago, you’ll need a booster before you travel.
It contains active ingredients to help your body develop an immunity to all three diseases. Don’t worry if you notice redness, swelling or soreness at the site of injection, as this is a common side effect. You may also feel unwell, experience nausea or develop a fever and headache shortly after the jab.
Revaxis is the combined Diphtheria, Tetanus and Polio Vaccine used by the Health Plus Pharmacy. It is specifically intended as a booster and should not be given as the primary course and/or to children under the age of 6. The diphtheria, tetanus & polio combined vaccine is a provided in a single injection. A booster is required every 10 years.
How the diphtheria, tetanus & polio vaccine is given?
The diphtheria, tetanus & polio vaccine is given as 1 separate injection, usually into the upper arm.
Diphtheria, tetanus & polio vaccination schedule
One booster dose. If you have never had the vaccine before you may need more than one dose.
You should get your diphtheria, tetanus & polio booster two weeks before travel.
How effective is the diphtheria, tetanus & polio vaccination
The diphtheria, tetanus & polio vaccine is very effective. The table below shows the average number of deaths in the UK each year, before and after introduction of a diphtheria, tetanus & polio vaccine:
| Disease | Before | After |
|---|---|---|
| Diphtheria | 3500 | 0 |
| Tetanus | 200 | 0 |
| Polio | 200 | 0 |
| Total | 3900 | 0 |
Source: Public Health England
Who should have the diphtheria, tetanus & polio vaccination
The diphtheria, tetanus & polio vaccine should form part of your childhood vaccination schedule, making it relevant for everyone.
Diphtheria, tetanus & polio is licenced from 6 years of age but it can be given from that age onwards including adults.
It is also considered a travel vaccine as adults who haven’t had their booster in the last 10 years will require a booster to top up their protection when traveling to high risk countries. Areas with a high incidence of polio and diphtheria include parts of Africa, Asia, Eastern Europe and the Middle East.
People travelling to these high risk countries should ensure their vaccinations are up-to-date before leaving. You should get your diphtheria, tetanus & polio booster two weeks before travel.
For up-to-date information about the area you’re visiting, check the TravelHealthPro country guides.
Who cannot have the diphtheria, tetanus & polio vaccine
Do not have the diphtheria, tetanus & polio vaccine jab if you have had a severe allergic reaction (anaphylaxis) to a previous dose or an ingredient in the vaccine.
If you’re ill with a fever postpone vaccination until you’re better. This is so any symptoms of an existing illness cannot be confused with an adverse reaction to the vaccine.
Monitoring vaccine safety
In the UK the Yellow Card Scheme allows doctors, other healthcare professionals, and you to report suspected side effects from any medicine you are taking, including vaccines.
It is run by the Medicines and Healthcare products Regulatory Agency (MHRA). The MHRA regularly reviews the yellow card reports. If it feels there is a potential problem, it will carry out an investigation and, if necessary, take appropriate action.
Most reactions reported through the Yellow Card Scheme have been minor reactions such as rashes, fever, vomiting, and redness and swelling where the injection was given.
There is also a legal requirement for pharmaceutical companies to report serious and suspected adverse events to the MHRA.
Find out how to report a vaccine side effect
What is diphtheria?
Diphtheria is a highly contagious infection that affects the nose and throat, and sometimes the skin. It’s rare in the UK, but there’s a small risk of catching it if you travel to some parts of the world.
It is spread via water droplets which can be transmitted through coughing, sneezing, sharing cups/cutlery, and close contact with someone who is infected. You can also become infected by sharing bedding or clothing with an infected person.
Diphtheria can be a serious illness and sometimes fatal, especially in children, if it’s not treated quickly. Vaccination can prevent it.
If you’re travelling to a part of the world where there may be a risk of diphtheria, you may need a booster vaccination if you were last vaccinated against it more than 10 years ago.
Since 2018, the World Health Organization has reported a rise in cases in places including:
- Indonesia
- India
- South America
- Africa
Places that have higher cases of diphtheria often change over time. For up-to-date information about the area you’re visiting, check the TravelHealthPro country guides.
What are the symptoms of diphtheria?
Symptoms usually start 2 to 5 days after becoming infected.
Symptoms of diphtheria include:
- a thick grey-white coating that may cover the back of your throat, nose and tongue
- a high temperature (fever)
- sore throat
- swollen glands in your neck
- difficulty breathing and swallowing
In countries with poor hygiene, infection of the skin (cutaneous diphtheria) is more common.
If it’s cutaneous diphtheria, it can cause:
- pus-filled blisters on your legs, feet and hands
- large ulcers surrounded by red, sore-looking skin
How serious diphtheria?
Diphtheria is a highly contagious infection that affects the nose and throat, and sometimes the skin. It’s rare in the UK, but there’s a small risk of catching it if you travel to some parts of the world.
Diphtheria can be a serious illness and sometimes fatal, especially in children, if it’s not treated quickly. Vaccination can prevent it.
Which countries are affected by diphtheria?
Diphtheria is common in many countries in Asia, the Middle East, eastern Europe, the Caribbean and the South Pacific (see map), while outbreaks have also been reported in other countries. The disease is more common in countries which do not offer routine vaccination.
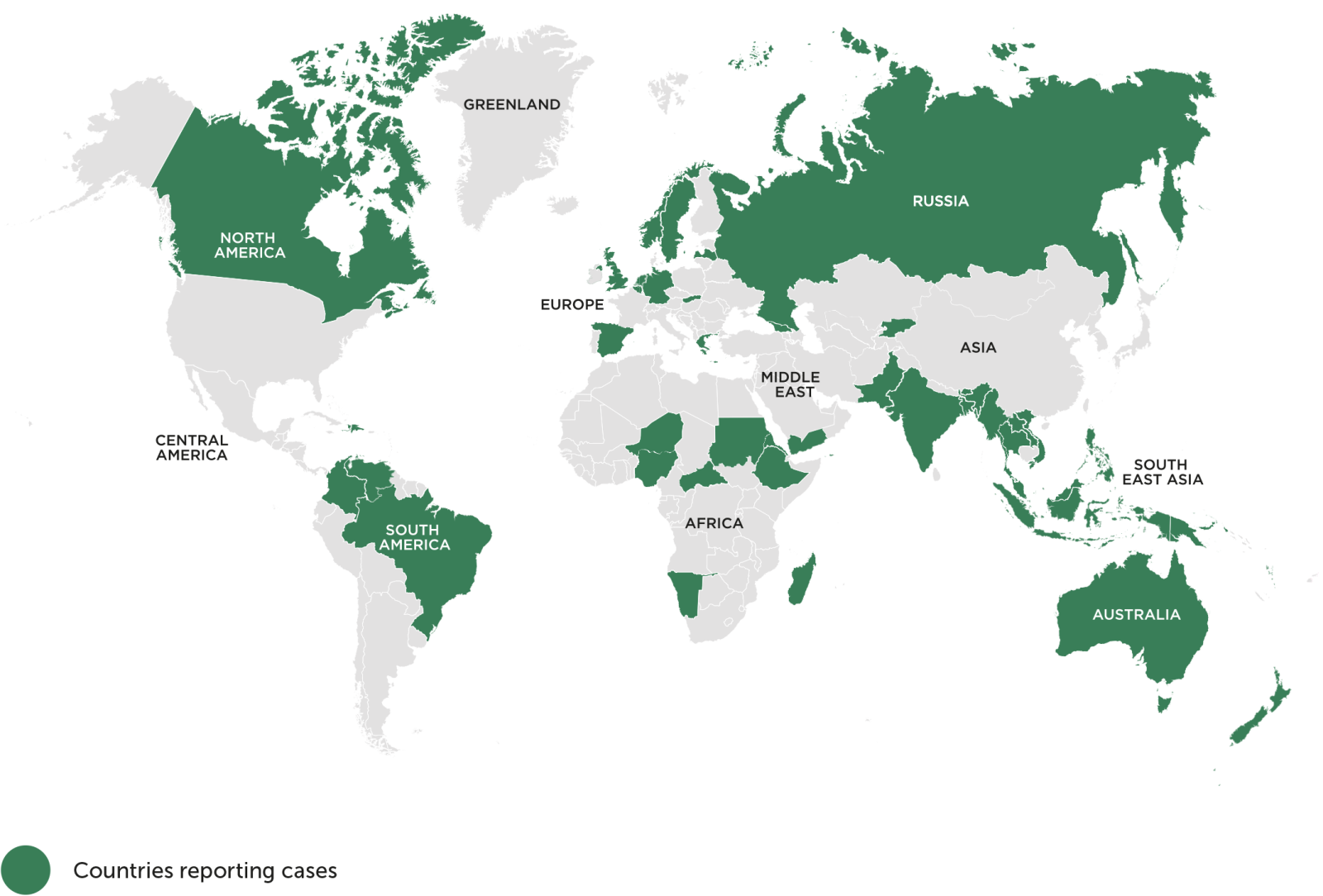
Map adapted from the World Health Organization. Immunization Monitoring. Diphtheria Reported Cases. October 2020.
What is tetanus?
Tetanus is a serious infection caused by bacteria getting into a wound.
The bacteria can enter the body through cuts and grazes, body piercings, tattoos and injections, burns, animals etc. Tetanus is fatal in around 1 in 10 cases.
Most people who get tetanus have either not been vaccinated against it or did not complete the entire vaccination schedule.
Tetanus bacteria can survive for a long time outside the body and are commonly found in soil and the manure of animals such as horses and cows.
If the bacteria enter the body through a wound they can quickly multiply and release a toxin that affects the nerves, causing symptoms such as muscle stiffness and spasms.
The bacteria can get into your body through:
- cuts and grazes
- tears or splits in the skin
- burns
- animal bites
- body piercings, tattoos and injections
- eye injuries
- injecting contaminated drugs
Tetanus cannot be spread from person to person.
What are the symptoms of tetanus?
The symptoms of tetanus usually start around 4 to 21 days after infection. On average, they start after around 10 days.
The main symptoms of tetanus include:
- stiffness in your jaw muscles (lockjaw), which can make it difficult to open your mouth
- painful muscle spasms, which can make it difficult to breathe and swallow
- a high temperature
- sweating
- a rapid heartbeat
If it’s not treated, the symptoms can get worse over the following hours and days.
Fast treatment is necessary to prevent symptoms from worsening and anyone developing symptoms of tetanus will usually need to be admitted to hospital.
How serious tetanus?
Tetanus is a serious but rare condition caused by bacteria getting into a wound. If you have signs or symptoms of tetanus, seek emergency care. If you have a simple, clean wound — and you’ve had a tetanus shot within 10 years — you can care for your wound at home.
Most people who get tetanus have either not been vaccinated against it or did not complete the entire vaccination schedule.
Tetanus is occasionally reported in England and Wales. Since 1991, there has been an average of seven cases reported each year; there have been no cases of neonatal tetanus in England and Wales for over 40 years. The majority of cases reported between 1984 and 2014 occurred in those over 45 years of age, many will have been born before routine vaccination schedules for tetanus were implemented in the UK in 1961.
In 2003, nine of the 12 reported cases occurred in people who inject drugs (PWID) aged between 20 and 47 years. Tetanus can be caused by contamination of drugs with spores during the production, distribution, storage, cutting, reconstitution and injection of drugs. Tetanus associated with foreign travel has only been reported twice in England and Wales since enhanced surveillance began in 1984.
The number is low because an effective tetanus vaccine is given as part of the NHS childhood vaccination programme.
Which countries are affected by tetanus?
Tetanus is found across the world, but some countries have higher incidences than others (see map).
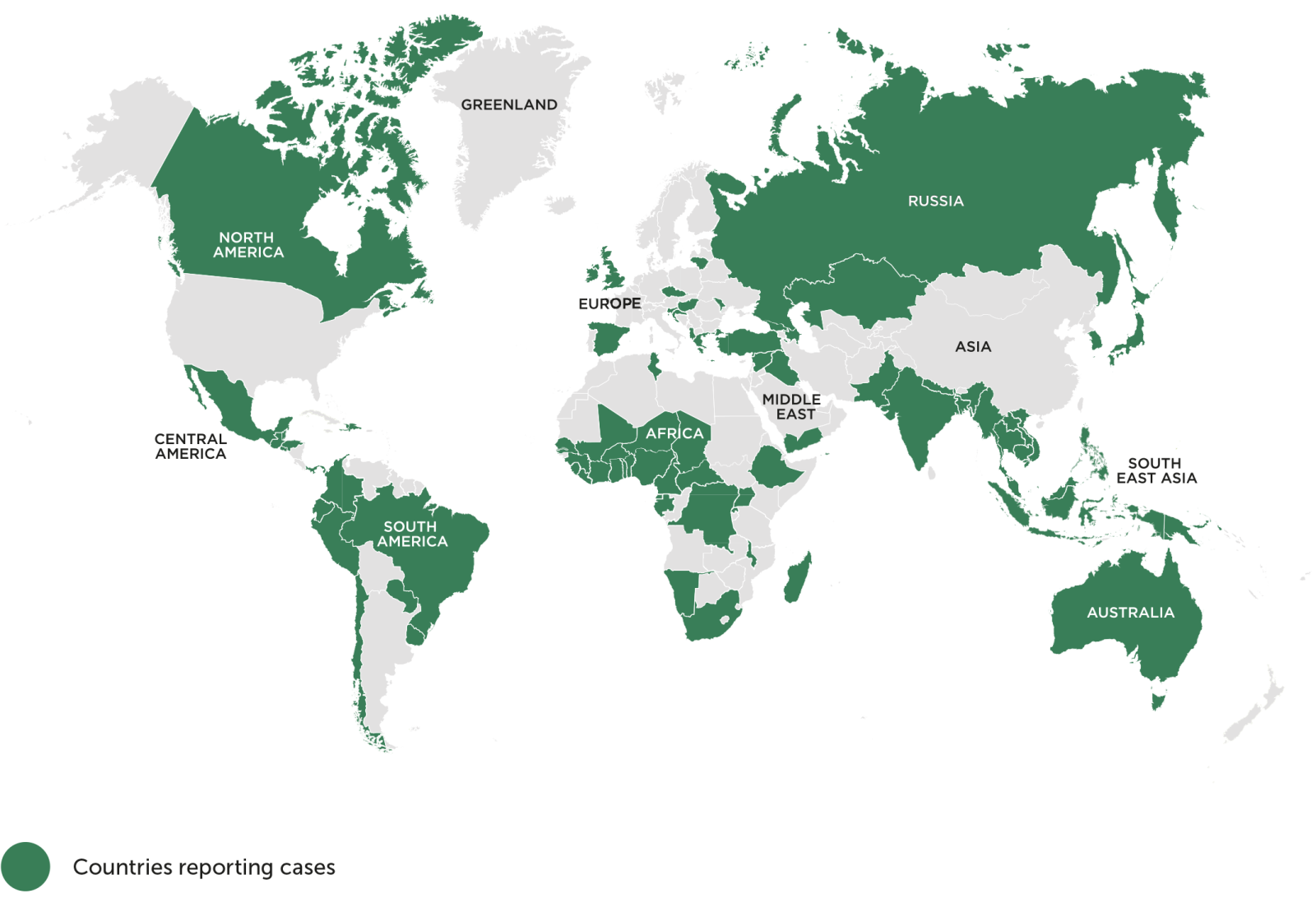
Map adapted from the World Health Organization. Immunization Monitoring. Tetanus (total) reported cases. October 2020.
What is polio?
Polio is caused by a virus that spreads easily from person to person.
It usually spreads through contact with the poo of an infected person. For example, from not washing your hands properly and putting them in your mouth, or from contaminated food or water.
It can also spread through coughs or sneezes, but this is less common.
Your chance of getting polio in the UK is extremely low. This is because most people are fully vaccinated. Polio was eradicated in Europe in 2003.
There’s still an extremely small risk of catching it when travelling in a country where polio is still found, such as Afghanistan and Pakistan.
If you’re not vaccinated, there is also a very small risk of getting it through contact with a person bringing the polio virus from these countries when they return to the UK.
In severe cases of polio, the virus can attack the nerves in the spine and brain which can cause paralysis. In some cases, it can cause persistent or lifelong difficulties and even be life threatening.
What are the symptoms of polio?
Most people won’t develop any symptoms of polio or even realise they’re infected.
Some people get mild, flu-like symptoms, such as:
- a high temperature
- extreme tiredness (fatigue)
- headaches
- being sick (vomiting)
- a stiff neck
- muscle pain
These symptoms usually last up to 10 days.
Rarely, polio can lead to more serious symptoms that affect the brain and nerves, such as weakness in your muscles (paralysis), usually in the legs. This can happen over hours or days.
If the paralysis affects the muscles used for breathing, it can be life threatening.
Most people will recover, and movement will slowly come back over the next few weeks. Some people can be left with permanent disability.
How serious polio?
Polio is a serious infection that’s now very rare because of the vaccination programme. It’s only found in a few countries and the chance of getting it in the UK is extremely low.
Rarely, polio can lead to more serious symptoms that affect the brain and nerves, such as weakness in your muscles (paralysis), usually in the legs. This can happen over hours or days. If the paralysis affects the muscles used for breathing, it can be life threatening.
Most people will recover, and movement will slowly come back over the next few weeks. Some people can be left with permanent disability.
Which countries are affected by polio?
Most countries are now free of polio (see map). The risk of polio is greatest in Afghanistan and Pakistan. Certain other countries are also affected.
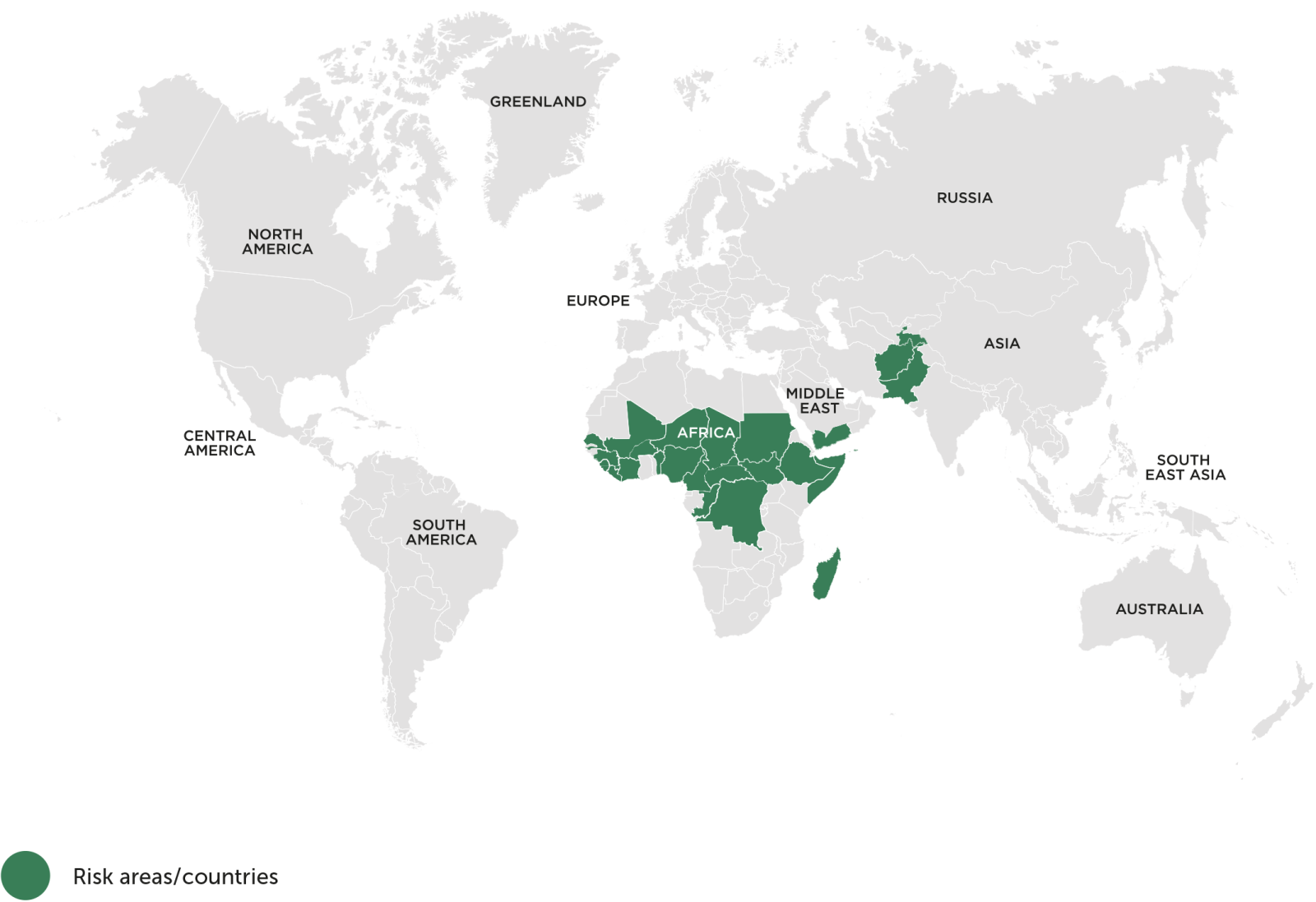
Map adapted from the World Health Organization. Factsheet. Poliomyelitis. July 2019.
If I was vaccinated against tetanus, diphtheria and polio as a child, am I still protected?
You’ll have some protection, but the diphtheria, tetanus & polio booster vaccination will strengthen this and help keep you protected for many more years.
How many boosters do I need to have?
In total, you need 5 doses of the tetanus, diphtheria and polio vaccines through your childhood. This will build up and maintain your body’s own immunity against these infections and protect you against the diseases.
You receive the first 3 doses as a baby in the 6-in-1 vaccine. The 4th dose is given around the age of 3 as a pre-school booster in the 4-in-1 vaccine, and the 5th and final dose is the diphtheria, tetanus & polio vaccine given at age 14 (school year 9).
You’ll usually only need an additional booster before travelling to some countries or if you have had a certain type of injury.
If you think you may have missed any of your doses, talk to a doctor, practice nurse or school nurse.
Should I have any other vaccinations at the same time as the diphtheria, tetanus & polio vaccination?
You’ll probably be offered the Meningitis ACWY vaccine at the same time as your diphtheria, tetanus & polio vaccine.
It’s also a good opportunity to check with the doctor or nurse that all your other vaccinations are up-to-date, such as MMR. If not, you can have these other routine childhood vaccinations at the same time as the diphtheria, tetanus & polio vaccine.


